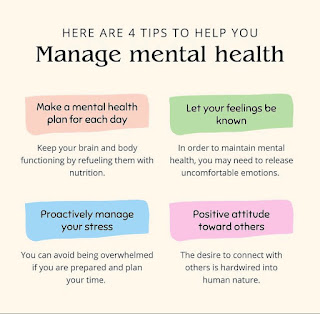
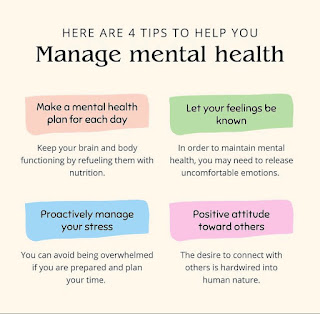
TIPS TO MANAGE MENTAL HEALTH
PARACETAMOL TOXICITY :
Metabolism:
the metabolism of
acetaminophen, identify the key toxic metabolite, describe the clinical
presentation of acetaminophen toxicity, and discuss the treatment and antidote
for acetaminophen toxicity. We will start with a general discussion about
acetaminophen and then talk about its pharmacology and metabolism and how this
applies
to acetaminophen
toxicity. We'll then discuss the clinical presentation and finally the
treatment for acetaminophen toxicity.
About Paracetamol:
Acetaminophen is one of
the most commonly used analgesics in antipyretics today.
It is in many
over-the-counter medications as well as in many prescription medications in
combination with various opioids.
Because of this, in
addition to acetaminophen toxicity, you must consider toxicity from other
medications in acute and chronic ingestions. Many consider acetaminophen to be
a benign medication. However, it is the most common cause of acute fulminate
liver
failure in the United
States.
Overdose:
In overdose, it can be
fatal, cause hepatic necrosis and fulminate liver failure that requires
transplantation.
Absorption:
Acetaminophen is rapidly
absorbed by the GI tract. 97% is metabolized by the liver, and the remaining 3%
is excreted
unchanged in the urine. Of
the 97% metabolized by the liver, 94% goes through either glucuronidation or
sulfation and then gets excreted in the urine.
The remaining 3% is
metabolized by the P450 system to a metabolite called NAPQI.
Cause of Toxicity:
This is the metabolite
that causes the heap toxicity seen in acetaminophen overdose. NAPQI is rapidly
metabolized by glutathione in the liver to non-toxic metabolites which get
excreted in the urine. When acetaminophen is ingested in large doses, the
metabolism of NAPQI depletes glutathione stores. When glutathione levels reach 30%
or less, the hepatotoxic effects of NAPQI begin to take place.
Precaution:
Patients with chronic
liver disease, malnutrition, or alcoholism are much more sensitive to the
effects of NAPQI. And hepatotoxicity can be seen
in lower-dose ingestions
of acetaminophen. This is mainly because these patients are deficient in
glutathione.
The clinical
presentation takes place in four stages.
Stage 1 presents with very nonspecific
constitutional and GI symptoms, which can make the diagnosis especially
challenging if the patient does not volunteer information on acetaminophen
ingestion. This stage lasts for up to 24
hours post-ingestion.
Stage 2, the hepatotoxic
effects of NAPQI BDN. Clinical hepatitis develops with rising liver enzymes, right
upper quadrant pain, and right upper quadrant tenderness on exam.
Typically, blood levels of
acetaminophen are low at this point, because it has been completely
metabolized. Serum drug
tests test only for acetaminophen and not the metabolites of acetaminophen. This
stage is seen between 24 hours and 48 hours post-ingestion.
Stage 3 is the point of maximum
toxicity. Liver enzymes peak at 10,000 to 20,000. Other causes of acute
hepatitis,
such as viruses and
alcohol, usually do not result in profound transaminitis like acetaminophen
toxicity. Other signs of liver failure also begin to appear, such as encephalopathy
or coagulopathy. This is typically seen on days 3 and 4 post-ingestion.
Stage 4 is either a recovery phase,
with the return of normal liver function and no long-term damage, or a stage where
patients go into fulminant hepatic failure and can require transplantation. This
stage lasts up to two weeks post-ingestion. Typically, acetaminophen toxicity
takes place in injections that are greater than 150 milligrams per kilogram in
children and greater than 7 and 1/2 to 10 grams in adults.
Treatment:
When deciding if
treatment with an N-acetylcysteine, which is the antidote, is necessary,
we use the
Rumack-Matthew nomogram. This nomogram is based on the acetaminophen level at
four hours or greater post-ingestion as well as the half-life of acetaminophen.
Luckily, acetaminophen overdose does have an antidote, which is the mainstay of
treatment.
This is
N-acetylcysteine or NAC for short. This is metabolized to precursor glutathione,
which can then be used to metabolize the toxic NAPQI. It is 100% effective if
given within eight hours of ingestion, making this diagnosis especially time-sensitive.
Gastric lavage and the use of ipecac to induce vomiting are no longer
recommended, mainly because of the risk of aspiration and causing pneumonitis. GI decontamination with activated charcoal can be used in large
ingestions if the patient presents within two hours. This is the Rumack-Matthew nomogram.
It is based on a level of
acetaminophen at four hours or greater and the half-life of acetaminophen. So
this nomogram is divided into three areas.
The area above line 1 represents
probable toxicity. If a patient falls above this line on their acetaminophen
level, they will likely go on to develop hepatotoxicity, and all these patients
should be started on NAC therapy.
The area below line 2 represents
no toxicity and patients that should not go on to develop hepatotoxicity from
NAPQI.
So these patients do not
need
to be treated.
Patient History:
Keep in mind that
patients with alcoholism, malnutrition and chronic liver disease can have
toxic ingestions at lower doses.
So, if those patients
are in the possible or probable toxicity levels, you might want also to still consider
treating them with an N-acetylcysteine.
So basically, NAC should
be administered in three situations.
Comments
Post a Comment